Link to document mentioned in video http://www.ncbi.nlm.nih.gov/pubmed/23696790


Link to document mentioned in video http://www.ncbi.nlm.nih.gov/pubmed/23696790

[svpVideo v=1]
Drug that steals women's lives: It's more addictive than heroin, with horrifying side-effects. So why, 50 years after its launch, is Valium still given to millions?
Read more: http://www.dailymail.co.uk/femail/article-2289311/Valium-Its-addictive-heroin-horrifying-effects-given-millions.html#ixzz4dEdqgVxF
Follow us: @MailOnline on Twitter | DailyMail on Facebook
Medicines and their possible side effects can affect individual people in different ways. The following are some of the side effects that are known to be associated with this medicine. Just because a side effect is stated here does not mean that all people using this medicine will experience that or any side effect.
Drowsiness, including drowsiness and lightheadedness the next day.
See warnings above.
Talk to your doctor, nurse or pharmacist if you want any more information about the possible side effects of this medicine. If you think you have experienced a side effect, did you know you can report this using the yellow card website?
How can I stop diazepam (Valium)?
Furthermore, “rebound symptoms” can occur, which may manifest in high levels of anxiety. However, these symptoms should begin to decline about 6-8 weeks after quitting Valium. 24 – 72 hours Valium withdrawal: Withdrawal from Valium mimics that of alcohol. Your body will experience tremors, sweating, and agitation
Short-term (two to four weeks only) treatment of severe anxiety that is disabling or subjecting the individual to unacceptable distress.
Short-term (two to four weeks only) treatment of severe insomnia that is disabling or subjecting the individual to extreme distress (oral forms of diazepam only).
Relieving anxiety and causing sedation before surgery or medical procedures (pre-med).
Managing symptoms of withdrawal from alcohol (used in combination with other treatment for alcoholism).
Controlling convulsions (fits) caused by poisoning (intravenous and rectal forms of diazepam only).
Controlling repeated fitting with no recovery of conciousness between seizures (status epilepticus) (intravenous and rectal forms of diazepam only).
Controlling fitting associated with fever (febrile convulsions).
Controlling muscle spasms, for example due to tetanus or poisoning.
Diazepam is a type of medicine called a benzodiazepine. Benzodiazepines are used for their sedative, anxiety-relieving and muscle-relaxing effects.
Diazepam works by acting on receptors in the brain called GABA receptors. This causes the release of a neurotransmitter called GABA in the brain.
Neurotransmitters are chemicals that are stored in nerve cells in the brain and nervous system. They are involved in transmitting messages between the nerve cells. GABA is a neurotransmitter that acts as a natural ‘nerve-calming' agent. It helps keep the nerve activity in the brain in balance, and is involved in inducing sleepiness, reducing anxiety and relaxing muscles.
As diazepam increases the activity of GABA in the brain, it increases its calming effect and results in sleepiness, a decrease in anxiety and relaxation of muscles.
Diazepam has several uses. Firstly, it can be used to calm severe anxiety and agitation. For example, benzodiazepines such as diazepam are effective at quickly reducing the symptoms of anxiety and agitation that occur in a manic episode of the psychiatric illness, bipolar affective disorder. A benzodiazepine may be given as part of the initial treatment of a manic episode, though they are not licensed specifically for this purpose. Benzodiazepines help calm the individual while the main medicines for this condition (mood stabilizers) begin to take effect.
Oral forms of diazepam are also used for short-term treatment of severe anxiety associated with insomnia. Diazepam decreases the time taken to fall asleep and wakings during the night, as well as increasing the total amount of time spent sleeping. However, it is only suitable for short-term treatment of insomnia and anxiety as it has a high potential for dependence and addiction. As diazepam remains active in the body for many hours, drowsiness may also last into the next day.
Diazepam is also given for its sedating and anxiety-relieving effects as a pre-med before surgery or medical investigations and procedures, and to alcoholics during acute alcohol withdrawal (‘cold-turkey').
The second main use of diazepam is in controlling convulsions, for example, associated with poisoning, or seizures associated with fever in children (febrile convulsions). It is particularly useful for controlling repeated epileptic fits when the person doesn't recover consciousness between fits (status epilepticus). Diazepam helps control convulsions because the increased activity of GABA that it causes in the brain helps to calm the excessive electrical nerve activity that is responsible for causing seizures.
A further use of diazepam is in controlling muscle spasms due to tetanus or poisoning.
Related Article
Treatments for anxiety
Diazepam may be taken as tablets or syrup, or given by injection or rectal solution (enema), depending on what condition is being treated and how fast a response is needed.
Diazepam tablets and syrup can be taken either with or without food.
Always take the medicine as directed by your doctor. Do not exceed the dose prescribed by your doctor.
Things you should know before taking Diazepam?
This medicine causes drowsiness and muscle weakness and impairs concentration and alertness. These effects may continue into the following day and are made worse by drinking alcohol. If you are affected you should not drive or operate machinery.Do not drink alcohol while taking this medicine.
From March 2015 a new ‘drug driving' law comes into force, which makes it an offence to drive with certain drugs or prescription medicines above specified limits in your body. The list includes diazepam, which means it may be an offence to drive while you are taking this medicine. The new law will allow police to use roadside drug tests to check for the presence of the prohibited drugs in a driver's saliva. There are very low limits for illegal drugs, but higher limits for prescribed medicines. This should mean that most people taking diazepam as prescribed will not be breaking the law, provided they are not driving dangerously. If you are found to be above the limit for diazepam there is a medical defence if you are taking the medicine as prescribed, as long as your driving is not impaired. If you are taking a high dose of diazepam it may therefore be sensible to carry your prescription with you when driving, in case you are asked to take a test by the police. However, if you are driving dangerously while taking this medicine you will be breaking the law. You should not drive if you think this medicine affects your ability to drive safely, for example if it makes you feel sleepy, dizzy, unable to concentrate or make decisions, or if you have blurred or double vision.
This medicine is generally only suitable for short-term use. If it is used for long periods or in high doses, tolerance to and physical and psychological dependence upon the medicine may develop, and withdrawal symptoms may occur if treatment is stopped suddenly.
Treatment with this medicine should usually be stopped gradually, following the instructions given by your doctor, in order to avoid withdrawal symptoms such as rebound insomnia or anxiety, confusion, sweating, tremor, loss of appetite, irritability or convulsions.
Children.
Elderly people.
Weak or debilitated people.
Decreased kidney function.
Decreased liver function.
People with disease affecting the airways or lungs (respiratory disease).
People with a history of alcoholism or drug abuse.
People with personality disorders.
Depression.
It is important to tell your doctor if you have recently suffered a loss or bereavement, for example the death of a close friend or relative, before taking this medicine. Benzodiazepines such as this one can affect the way you adjust psychologically to events like this.
People who are allergic to other benzodiazepines.
People with a sudden worsening of any underlying lung disease (acute pulmonary insufficiency).
People with slow, shallow breathing (respiratory depression).
People who suffer from sleep apnoea syndrome, which is a problem involving short spells when breathing stops during sleep.
People with abnormal muscle weakness due to the condition myasthenia gravis.
Long-term psychotic illness.
Phobias or obsessional states.
People who are very restless or hyperactive.
Severely decreased liver function.
Breastfeeding.
This medicine should not be used if you are allergic to one or any of its ingredients. Please inform your doctor or pharmacist if you have previously experienced such an allergy.
If you feel you have experienced an allergic reaction, stop using this medicine and inform your doctor or pharmacist immediately.
Can I take Diazepam while pregnant or breastfeeding?
Certain medicines should not be used during pregnancy or breastfeeding. However, other medicines may be safely used in pregnancy or breastfeeding providing the benefits to the mother outweigh the risks to the unborn baby. Always inform your doctor if you are pregnant or planning a pregnancy, before using any medicine.
This medicine may be harmful to a developing baby and it should be avoided during pregnancy unless considered essential by your doctor. This is particularly important during the first and third trimesters of pregnancy and before or during labour. Regular use during pregnancy should especially be avoided, as the baby could become dependent on the medicine and then suffer withdrawal symptoms after the birth. If this medicine is used in late pregnancy or during labour it may cause floppiness, low body temperature and breathing or feeding difficulties in the baby after birth. Ask your doctor for further information.
Significant amounts of this medicine may pass into breast milk. It should not be used by breastfeeding mothers as it may be harmful to the nursing infant. Seek medical advice from your doctor.
Related Article
Over-the-counter medicines in pregnancy
ADVERTISEMENT – CONTINUE READING BELOW
It is important to tell your doctor or pharmacist what medicines you are already taking, including those bought without a prescription and herbal medicines, before you start treatment with this medicine. Similarly, check with your doctor or pharmacist before taking any new medicines while taking this one, to make sure that the combination is safe.
Related Article
Is it dangerous to take different medicines at the same time?
There may be an increased risk of drowsiness and sedation if diazepam is taken with any of the following (which can also cause drowsiness):
alcohol
antipsychotics, eg chlorpromazine, clozapine
antipsychotics, eg chlorpromazine, clozapine
baclofen
baclofen
barbiturates, eg phenobarbital
barbiturates, eg phenobarbital
other benzodiazepines, eg temazepam
other benzodiazepines, eg temazepam
lofexidine
lofexidine
MAOI antidepressants, eg phenelzine
MAOI antidepressants, eg phenelzine
nabilone
nabilone
sedating antihistamines, eg chlorphenamine
sedating antihistamines, eg chlorphenamine
sleeping tablets, eg zopiclone
sleeping tablets, eg zopiclone
strong opioid painkillers, eg morphine, codeine, dihydrocodeine
tizanidine
tricyclic antidepressants, eg amitriptyline.
The following medicines may prevent the breakdown of diazepam in the body. As this could increase the blood level of diazepam and its sedative effects, as well as the risk of its side effects, your doctor may need to prescribe you a lower than normal dose of diazepam if you are taking any of these medicines:
cimetidine
disulfiram
esomeprazole
fluconazole
fluoxetine
fluvoxamine
fosamprenavir
isoniazid
itraconazole
ketoconazole
modafinil
oestrogens and progestogens, for example in contraceptives like the pill
omeprazole
ritonavir (diazepam should preferably not be used in people taking ritonavir)
valproate
voriconazole.
Diazepam may enhance the blood pressure lowering effect of medicines that lower blood pressure, particularly medicines used to treat high blood pressure (antihypertensives), diuretic medicines and nitrates for angina. This may cause dizziness, which can usually be relieved by lying down until the symptoms pass.
The following medicines may decrease the blood level of diazepam. As this could make it less effective, your doctor may need to prescribe you a larger than normal dose of diazepam if you are taking any of these medicines:
phenytoin
rifampicin.
Caffeine and theophylline may reduce the sedative and anxiety-reducing effects of diazepam.
Diazepam may reduce the effectiveness of levodopa in treating Parkinson's disease.
Diazepam may increase or decrease blood levels of the anticonvulsant medicine phenytoin.
People who break free from benzodiazepine addictions tend to feel a lot better: Studies show that quitting leads to improvements in cognitive performance, mood and sleeping, and since the prolonged use of a benzodiazepine often causes as many anxiety problems as it’s supposed to solve, quitting generally makes very good sense.
But though quitting is sensible, it’s certainly not easy,especially if you don’t start with a reasonable understanding of the process and a solid plan for success.
So read on to learn more about…
Not everyone quitting benzos will experience withdrawal symptoms and most people experience only a few, not the complete list of possible symptoms.
Typical withdrawal symptoms include:1
See the end of this article for a comprehensive list of less commonly experienced withdrawal symptoms.
All benzodiazepines work by increasing the activity of the neurotransmitter GABA. Since GABA is an inhibitory transmitter, which slows or stops the firing of other neurotransmitters, by increasing GABA activity you quiet the brain’s overall activity level. GABA is the brain’s natural sedative, and benzodiazepines simply enhance its functioning.
GABA suppresses excitatory neurotransmitters like dopamine, serotonin, epinephrine (noradrenaline) and acetylcholine. These excitatory transmitters play important roles in memory, muscle movement, alertness, emotional regulation, heart rate and blood pressure and hormonal secretions. When taking benzodiazepines you quiet your whole brain’s activity level. This reduces anxiety and insomnia, but also causes changes to many of the body’s essential systems. This is why taking chronic high doses of benzos can cause such a variety of health problems and why people experience such a wide array of withdrawal symptoms after stopping.
Benzodizepine users quickly develop a tolerance and start needing increasingly larger doses to achieve any desired effects. Because of this, most prescribing guidelines advise against the use of benzos for more than 3 or 4 consecutive weeks.
With tolerance:
So once you’ve developed a tolerance you need large doses of benzos to just get the GABA system functioning at a ‘normal’ level. If a person with a benzo tolerance suddenly stops taking their medication, GABA activity drops substantially and this causes equally substantial increases in the activity of the brain's excitatory dopamine, serotonin, noradrenalin etc. systems.2
In some cases, as your tolerance rises, you can start to experience withdrawal symptoms on a steady dose, and you need to up your daily dosage to keep these withdrawal symptoms at bay.
According to the benzodiazepine dependency advocacy group Reconnexion, between 50% and 80% of people who use benzos for 6 months or longer will experience at least some withdrawal symptoms after stoppage.
The duration of withdrawal symptoms can also vary a great deal, but people who have longer histories of use are more likely to experience longer withdrawal periods than people with shorter use histories.3
You are more likely to have difficult withdrawal symptoms when quitting:4
You will start to feel withdrawal symptoms sooner if using a shorter acting benzo, like Xanax, and later, if using a long acting benzo, like valium.
Withdrawal symptoms may persist for a few days or weeks. Some people experience withdrawal symptoms that persist for months or even years after cessation of use.
Taper. Without a doubt.
If you have been using benzodiazepines on a daily basis for more than three weeks, you should not stop using suddenly – you need to taper down instead.
You may have an impulse to try to power through quickly and tough it out. Although this is understandable – it's a very bad idea.
Tapering should be slow and gradual (months, not weeks) – it doesn’t really matter how long it takes (it probably took you a long time to build up your tolerance) and what’s most important is making steady progress towards your goal while minimizing your discomfort along the way (see below for example tapering schedules).
By tapering you can
You can do:
Many clinicians recommend switching to diazepam prior to initiating a tapering program.
Because of diazepam’s long half-life, and difficulties in finding exact equivalent dosages between benzos, it is generally recommended that you switch over to diazepam gradually, in a step-wise fashion over a period of weeks, and then once stable on diazepam, start your tapering from there.7
Because of the wide variations in half-life and thus variations in how people respond to different benzodiazepines (influenced by factors such as age and hepatic impairment) it’s quite difficult to provide an exactly equivalent diazepam to other benzodiazepine dosage.
According to the Victorian (Australia) Gov. drug withdrawal practice guidelines, as of 2009, 5 mgs of diazepam was approximately equivalent to:8
So, for example, if you wanted to switch from 2mgs of Xanax to an equivalent amount of diazepam you would need to take 20 mgs of diazepam.
Or, a more aggressive approach, endorsed by the Oregon State College of Pharmacy10
As a general rule, it doesn’t really matter how slowly you taper and it’s a good idea to stabilize at a dosage before moving further down. Reductions tend to get harder in the second half of the process, so it’s OK to slow down as you need to, as you approach the finish line.
However, you should definitely avoid:
Drinking may worsen your withdrawal symptoms (especially the morning after) but there’s another important reason to avoid alcohol until you feel better.
And if you do this, at the end of it all not only is your GABA system still out of whack – now you’ve got an alcohol problem too!
To minimize your symptoms:12
Staying focused on how bad you’re feeling won’t help you feel better, and the more you obsess about your symptoms, the worse you’ll perceive those symptoms to be – in fact, sometimes worrying about how you’ll feel after dose reductions causes more negative symptoms than the dose reduction itself!13
One trick you can use to minimize the worry is to accept that after each dose reduction you might catch a touch of ‘Benzo Flu’
Think objectively about how you feel after a dose reduction and compare these symptoms to how you feel when you catch a cold or flu. Are they comparable? When you get a flu do you worry a lot about how terrible you’re feeling or do you just accept that you’ll feel crummy for a few days and that you’ll feel better in time.
With benzo withdrawal symptoms it’s pretty much the same thing. You may feel crummy for a short time after a dose reduction, but you’ll feel better quickly enough, so why not just think of your symptoms as a case of benzo flu – and since you know that this flu will pass quickly enough, you don’t need to get too stressed about how bad you feel.
You should, ideally, seek a doctor’s medical supervision to help you with the withdrawal process, but on top of this, should you also seek out some form of counseling support?
Anxiety is the most commonly experienced benzo withdrawal symptom. This anxiety is temporary and will go away as your body readjusts, but if you find it very uncomfortable you may find counseling helpful.
Basically, this is a tough process, and if you’re having trouble coping with your withdrawal symptoms, it’s entirely reasonable to seek out extra helpful support and advice.
Your doctor may prescribe you medications that can reduce the severity of some withdrawal symptoms. Medications sometimes prescribed include:14
In addition to the more commonly experienced withdrawal symptoms from the list above, some people may experience one or more of the following:15

[svpVideo v=1]
[svpVideo v=2]
Like all medicines, even a single dose of Zithromax can trigger side effects, some of which may include:

[svpVideo v=1]
Neulasta may cause serious side effects, including:
Increased white blood cell count (leukocytosis). Your healthcare provider will check your blood during treatment with Neulasta.
Neulasta is a man-made form of granulocyte colony-stimulating factor (G-CSF). G-CSF is a substance produced by the body. It stimulates the growth of neutrophils, a type of white blood cell important in the body’s fight against infection. Acute Radiation Syndrome: The effectiveness of Neulasta for this use was only studied in animals, because it could not be studied in people.
Please download the Patient Product Information
Manufacturer Website for Neulasta

This drug is a highly addictive semisynthetic opioid. By modifying a plant-based drug used for centuries,
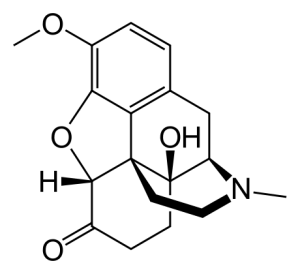
the pharmaceutical industry has been able to create a substance many times as addictive as the original formula. If you are currently taking this drug you will be facing a challenge to get off it.
You can manage pain with coffee enemas (up to five per day) as you reduce very gradually the drugs.
Oxycodone is a semisynthetic opioid synthesized from thebaine, an opioid alkaloid found in the Persian poppy, and one of the many alkaloids found in the opium poppy. It is a moderately potent opioid analgesic, generally indicated for relief of moderate to severe pain. Oxycodone was developed in 1917 in Germany] as one of several semi-synthetic opioids in an attempt to improve on the existing opioids.
Oxycodone is available as single-ingredient medication in immediate release and controlled release.
Oxycodone is metabolized by the enzymes CYP3A4 and CYP2D6, and its clearance therefore can be altered by inhibitors and inducers of these enzymes.[26] Natural genetic variation in these enzymes can also influence the clearance of oxycodone, which may be related to the wide inter-individual variability in its half-life and potency.[26]
Ritonavir or lopinavir/ritonavir greatly increase plasma concentrations of oxycodone in healthy human volunteers due to inhibition of CYP3A4 and CYP2D6. Rifampicin greatly reduces plasma concentrations of oxycodone due to strong induction of CYP3A4. There is also a case report of fosphenytoin, a CYP3A4 inducer, dramatically reducing the analgesic effects of oxycodone in a chronic pain patient. Dosage or medication adjustments may be necessary in each case.]
(For lists of CYP3A4 and CYP2D6 inhibitors and inducers, see here and here, respectively.)
Link over to Wikipedia for a big document on the drug
Major Side Effects
If any of the following side effects occur while taking oxycodone, check with your doctor immediately:
Less common:
Some oxycodone side effects may not need any medical attention. As your body gets used to the medicine these side effects may disappear. Your health care professional may be able to help you prevent or reduce these side effects, but do check with them if any of the following side effects continue, or if you are concerned about them:
these side effects may disappear. Your health care professional may be able to help you prevent or reduce
these side effects, but do check with them if any of the following side effects continue, or if you are concerned about them:
More common: Difficulty having a bowel movement (stool)
Difficulty having a bowel movement (stool)
drowsiness
lack or loss of strength
relaxed and calm feeling
sleepiness or unusual drowsiness

Allergic reaction: Itching or hives, swelling in your face or hands, swelling or tingling in your mouth or throat, chest tightness, trouble breathing
Blistering, peeling, red skin rash
Chest pain, shortness of breath
Confusion, weakness, muscle twitching
Dry mouth, increased thirst, muscle cramps, nausea or vomiting, uneven heartbeat
Sudden and severe stomach pain, nausea, vomiting, fever, lightheadedness
Hearing loss, ringing in the ears
Lightheadedness, dizziness, fainting
Severe diarrhea
Unusual bleeding or bruising
Yellow skin or eyes
Loss of appetite, stomach cramps
If you notice other side effects that you think are caused by this medicine, tell your doctor.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
Get emergency help immediately if any of the following symptoms of overdose occur:
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.

Flonase (fluticasone) is a synthetic steroid of the glucocorticoid family of drugs and is prescribed for the control of symptoms of allergic and non-allergic rhinitis. Flonase is available as a generic drug, and dosing is usually administered as two sprays in each nostril once daily, or one spray in each nostril twice daily.
The most common side effects of Flonase (fluticasone) include:
Flonase has also been associated with hypersensitivity reactions (for example, skin rash, itching, facial swelling, and anaphylaxis).
The recommended starting dosage of Flonase in adults is 2 sprays (50 mcg of fluticasone propionate each) in each nostril once daily (total daily dose, 200 mcg). Drug interactions and warnings include Norvir (ritonavir) and Nizoral (ketoconazole). Taking either one of these drugs with Flonase may increase the blood concentrations of Flonase and potentially increase its side effects. Flonase should only be used during pregnancy when it is absolutely necessary. There have not been adequate studies of Flonase and concentrations in breast milk; therefore, Flonase should be avoided while breastfeeding unless it is absolutely necessary.
Our Flonase Side Effects Drug Center provides a comprehensive view of available drug information on the potential side effects when taking this medication.
FLONASE® Allergy Relief is meant to work in your nose. Never use in your eyes or mouth.
If you or your child have an allergic reaction to this product, with sudden swelling of the face or tongue, a rash, or wheezing or feeling faint, stop using FLONASE® Allergy Relief and see a doctor right away.
If you or your child experiences a nose injury with severe or frequent nosebleeds, apply pressure to your nose. Stop using FLONASE® Allergy Relief and see a doctor right away.
If you or your child experiences a constant whistling sound that does not go away, this could be a sign of damage to your nose. Stop using FLONASE® Allergy Relief and see a doctor right away.
If you or your child experiences cloudy or reduced vision, it could be the result of eye conditions such as cataracts or glaucoma. Be sure to schedule a yearly eye exam to check for these conditions.
If administering to your child, talk to their pediatrician if you are concerned they may experience certain growth effects, such as a slower growth rate as a result of using FLONASE® Allergy Relief. Also, speak to your doctor if your child is between the ages of 4 and 11 needs to use FLONASE® Allergy Relief for longer than 2 months a year.
Talk to your doctor or pharmacist if you or your child experiences other side effects such as headaches or sneezing, a bad taste or smell, minor nosebleeds, or a dry or irritated nose or throat.
Finally, please read the Drug Facts on the back of the FLONASE® Allergy Relief or package to be aware of any additional information that may be helpful to you. If you have any concerns about side effects, talk to your doctor.
Use as directed. Please see specific products for full labeling information.

Morphine is an extremely addictive painkiller. In fact, morphine addictive properties make it a Schedule II narcotic under the Controlled Substances Act. When addicts try to quit morphine, they often experience severe cramps, pains and anxiety which can result in using the drug again in order to avoid withdrawal. But what are some clear signs of morphine addiction?
Here, we will explore the signs and symptoms of morphine addiction and let you know what you can do to help someone who is addicted. Then, we invite your questions about treating morphine addiction in the comments section at the end.
Morphine addiction can start as a prescribed medication to solve real pain issues. However, having morphine in the system can lead to habitual drug seeking or using morphine other than intended. Many users find that they cannot stop after even a few weeks of regular dosing.
Morphine addiction can result in a range of symptoms from weight loss to vomiting and memory problems. There are also obvious emotional signs of morphine addiction which can include anxiety, hallucinations, depression and irritability. Morphine addiction also reduces the addict’s level of consciousness, which affects their ability to be fully aware of their surroundings.
In addition to morphine withdrawal symptoms after a missed dose (lack of appetite, irritability, weight loss, drowsiness and sweating), Diagnostic and Statistical Manual of Mental Disorders clinical criteria for morphine addiction include:
I recomend gradual reduction with many coffee enemas, below ar the standard methods.
Morphine addiction symptoms can be treated through several different types of therapies and/or the use of prescription medications.
Psychological treatments – Psychotherapy and behavioral therapy are two of the most successful interventions for morphine addiction. These treatments address the emotional and cognitive aspects of addiction to resolve and change past behaviors.
Opiate replacement therapy – Replacement therapy attempts to curb addiction to morphine by replacing morphine with a less euphoric opioid, such as methadone or buprenorphine, which is taken under medical supervision. Replacement therapy helps addicts to lead a normal life while being treated with a substance that stops them from experiencing the harsh morphine withdrawal symptoms and cravings.
Prescription medications – There are medications available for morphine addiction and when used in combination with behavioral treatment programs increase chances of quitting morphine significantly. Prescription medications include anti-anxiety meds, antidepressants, and drugs such as nalexone or buprenorphine used to address withdrawal symptoms. Patients are less likely to become dependent on buprenorphine and when they stop the withdrawal symptoms are much weaker.
Morphine addiction support groups – Morphine addiction support groups can be useful for helping treat morphine addiction symptoms. Many addicts can find a sense of community by joining a support group and get further assistance psychologically months down the road to help prevent relapse. Support groups can be found at your local rehab center.

Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled studies of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled studies in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term studies of 9 antidepressant drugs in over 4,400 patients. The pooled analyses of placebo-controlled studies in adults with MDD or other psychiatric disorders included a total of 295 short-term studies (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs. placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1,000 patients treated) are provided in Table 1.
| Age Range | Drug-Placebo Difference in Number of Cases of Suicidality per 1,000 Patients Treated |
|---|---|
| Increases Compared to Placebo | |
| <18 | 14 additional cases |
| 18 to 24 | 5 additional cases |
| Decreases Compared to Placebo | |
| 25 to 64 | 1 fewer case |
| ?65 | 6 fewer cases |
No suicides occurred in any of the pediatric studies. There were suicides in the adult studies, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance studies in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that abrupt discontinuation can be associated with certain symptoms [see Dosage and Administration (2.4) and Warnings and Precautions (5.7) for a description of the risks of discontinuation of PRISTIQ].
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers. Such monitoring should include daily observation by families and caregivers.
Prescriptions for PRISTIQ should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Screening patients for bipolar disorder
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled studies) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that PRISTIQ is not approved for use in treating bipolar depression.
The development of a potentially life-threatening serotonin syndrome has been reported with SNRIs and SSRIs, including PRISTIQ, alone but particularly with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John's Wort), and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome.
The concomitant use of PRISTIQ with MAOIs intended to treat psychiatric disorders is contraindicated. PRISTIQ should also not be started in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. All reports with methylene blue that provided information on the route of administration involved intravenous administration in the dose range of 1 mg/kg to 8 mg/kg. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection) or at lower doses. There may be circumstances when it is necessary to initiate treatment with a MAOI such as linezolid or intravenous methylene blue in a patient taking PRISTIQ. PRISTIQ should be discontinued before initiating treatment with the MAOI [see Contraindications (4.2) and Dosage and Administration (2.6)].
If concomitant use of PRISTIQ with other serotonergic drugs, including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, amphetamines, tryptophan, and St. John's Wort is clinically warranted, patients should be made aware of a potential increased risk for serotonin syndrome, particularly during treatment initiation and dose increases.
Treatment with PRISTIQ and any concomitant serotonergic agents should be discontinued immediately if the above events occur and supportive symptomatic treatment should be initiated.
Patients receiving PRISTIQ should have regular monitoring of blood pressure since increases in blood pressure were observed in clinical studies [see Adverse Reactions (6.1)]. Pre-existing hypertension should be controlled before initiating treatment with PRISTIQ. Caution should be exercised in treating patients with pre-existing hypertension, cardiovascular, or cerebrovascular conditions that might be compromised by increases in blood pressure. Cases of elevated blood pressure requiring immediate treatment have been reported with PRISTIQ.
Sustained blood pressure increases could have adverse consequences. For patients who experience a sustained increase in blood pressure while receiving PRISTIQ, either dose reduction or discontinuation should be considered [see Adverse Reactions (6.1)].
SSRIs and SNRIs, including PRISTIQ, may increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs, warfarin, and other anticoagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to SSRIs and SNRIs have ranged from ecchymosis, hematoma, epistaxis, and petechiae to life-threatening hemorrhages. Patients should be cautioned about the risk of bleeding associated with the concomitant use of PRISTIQ and NSAIDs, aspirin, or other drugs that affect coagulation or bleeding.
Angle-Closure Glaucoma: The pupillary dilation that occurs following use of many antidepressant drugs including Pristiq may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
During all MDD phase 2 and phase 3 studies, mania was reported for approximately 0.02% of patients treated with PRISTIQ. Activation of mania/hypomania has also been reported in a small proportion of patients with major affective disorder who were treated with other marketed antidepressants. As with all antidepressants, PRISTIQ should be used cautiously in patients with a history or family history of mania or hypomania.
Discontinuation symptoms have been systematically and prospectively evaluated in patients treated with PRISTIQ during clinical studies in Major Depressive Disorder. Abrupt discontinuation or dose reduction has been associated with the appearance of new symptoms that include dizziness, nausea, headache, irritability, insomnia, diarrhea, anxiety, fatigue, abnormal dreams, and hyperhidrosis. In general, discontinuation events occurred more frequently with longer duration of therapy.
During marketing of SNRIs (Serotonin and Norepinephrine Reuptake Inhibitors), and SSRIs (Selective Serotonin Reuptake Inhibitors), there have been spontaneous reports of adverse events occurring upon discontinuation of these drugs, particularly when abrupt, including the following: dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesia, such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. While these events are generally self-limiting, there have been reports of serious discontinuation symptoms.
Patients should be monitored for these symptoms when discontinuing treatment with PRISTIQ. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose, but at a more gradual rate [see Dosage and Administration (2.4) and Adverse Reactions (6.1)].
Cases of seizure have been reported in pre-marketing clinical studies with PRISTIQ. PRISTIQ has not been systematically evaluated in patients with a seizure disorder. Patients with a history of seizures were excluded from pre-marketing clinical studies. PRISTIQ should be prescribed with caution in patients with a seizure disorder.
Hyponatremia may occur as a result of treatment with SSRIs and SNRIs, including PRISTIQ. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/L have been reported. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also, patients taking diuretics or who are otherwise volume depleted can be at greater risk [see Use in Specific Populations (8.5) and Clinical Pharmacology (12.6)]. Discontinuation of PRISTIQ should be considered in patients with symptomatic hyponatremia and appropriate medical intervention should be instituted.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which can lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death.
Interstitial lung disease and eosinophilic pneumonia associated with venlafaxine (the parent drug of PRISTIQ) therapy have been rarely reported. The possibility of these adverse events should be considered in patients treated with PRISTIQ who present with progressive dyspnea, cough, or chest discomfort. Such patients should undergo a prompt medical evaluation, and discontinuation of PRISTIQ should be considered.
The following adverse reactions are discussed in greater detail in other sections of the label.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in clinical practice.
Patient exposure
PRISTIQ was evaluated for safety in 8,394 patients diagnosed with major depressive disorder who participated in multiple-dose pre-marketing studies, representing 2,784 patient-years of exposure. Of the total 8,394 patients exposed to at least one dose of PRISTIQ; 2,116 were exposed to PRISTIQ for 6 months, representing 1,658 patient-years of exposure, and 421 were exposed for one year, representing 416 patient-years of exposure.
Adverse reactions reported as reasons for discontinuation of treatment
In the pre-marketing pooled 8-week placebo-controlled studies in patients with MDD, 1,834 patients were exposed to PRISTIQ (50 to 400 mg). Of the 1,834 patients, 12% discontinued treatment due to an adverse reaction, compared with 3% of the 1,116 placebo-treated patients. At the recommended dose of 50 mg, the discontinuation rate due to an adverse reaction for PRISTIQ (4.1%) was similar to the rate for placebo (3.8%). For the 100 mg dose of PRISTIQ the discontinuation rate due to an adverse reaction was 8.7%.
The most common adverse reactions leading to discontinuation in at least 2% and at a rate greater than placebo of the PRISTIQ treated patients in the short-term studies, up to 8 weeks, were: nausea (4%); dizziness, headache and vomiting (2% each). In a longer-term study, up to 9 months, the most common was vomiting (2%).
Common adverse reactions in placebo-controlled MDD studies
The most commonly observed adverse reactions in PRISTIQ treated MDD patients in pre-marketing pooled 8-week, placebo-controlled, fixed-dose studies (incidence ? 5% and at least twice the rate of placebo in the 50 or 100 mg dose groups) were: nausea, dizziness, insomnia, hyperhidrosis, constipation, somnolence, decreased appetite, anxiety, and specific male sexual function disorders.
Table 2 shows the incidence of common adverse reactions that occurred in ? 2% of PRISTIQ treated MDD patients and twice the rate of placebo at any dose in the pre-marketing pooled 8-week, placebo-controlled, fixed dose clinical studies
| Percentage of Patients Reporting Reaction | |||||
|---|---|---|---|---|---|
| PRISTIQ | |||||
| System Organ Class Preferred Term |
Placebo (n=636) |
50 mg (n=317) |
100 mg (n=424) |
200 mg (n=307) |
400 mg (n=317) |
| Cardiac disorders | |||||
| Blood pressure increased | 1 | 1 | 1 | 2 | 2 |
| Gastrointestinal disorders | |||||
| Nausea | 10 | 22 | 26 | 36 | 41 |
| Dry mouth | 9 | 11 | 17 | 21 | 25 |
| Constipation | 4 | 9 | 9 | 10 | 14 |
| Vomiting | 3 | 3 | 4 | 6 | 9 |
| General disorders and administration site conditions | |||||
| Fatigue | 4 | 7 | 7 | 10 | 11 |
| Chills | 1 | 1 | <1 | 3 | 4 |
| Feeling jittery | 1 | 1 | 2 | 3 | 3 |
| Metabolism and nutrition disorders | |||||
| Decreased appetite | 2 | 5 | 8 | 10 | 10 |
| Nervous system disorders | |||||
| Dizziness | 5 | 13 | 10 | 15 | 16 |
| Somnolence | 4 | 4 | 9 | 12 | 12 |
| Tremor | 2 | 2 | 3 | 9 | 9 |
| Disturbance in attention | <1 | <1 | 1 | 2 | 1 |
| Psychiatric disorders | |||||
| Insomnia | 6 | 9 | 12 | 14 | 15 |
| Anxiety | 2 | 3 | 5 | 4 | 4 |
| Nervousness | 1 | <1 | 1 | 2 | 2 |
| Abnormal dreams | 1 | 2 | 3 | 2 | 4 |
| Renal and urinary disorders | |||||
| Urinary hesitation | 0 | <1 | 1 | 2 | 2 |
| Respiratory, thoracic and mediastinal disorders | |||||
| Yawning | <1 | 1 | 1 | 4 | 3 |
| Skin and subcutaneous tissue disorders | |||||
| Hyperhidrosis | 4 | 10 | 11 | 18 | 21 |
| Special Senses | |||||
| Vision blurred | 1 | 3 | 4 | 4 | 4 |
| Mydriasis | <1 | 2 | 2 | 6 | 6 |
| Vertigo | 1 | 2 | 1 | 5 | 3 |
| Tinnitus | 1 | 2 | 1 | 1 | 2 |
| Dysgeusia | 1 | 1 | 1 | 1 | 2 |
| Vascular disorders | |||||
| Hot flush | <1 | 1 | 1 | 2 | 2 |
Sexual function adverse reactions
Table 3 shows the incidence of sexual function adverse reactions that occurred in ? 2% of PRISTIQ treated MDD patients in any fixed-dose group (pre-marketing pooled 8-week, placebo-controlled, fixed -dose, clinical studies).
| PRISTIQ | |||||
| Placebo (n=239) |
50 mg (n=108) |
100 mg (n=157) |
200 mg (n=131) |
400 mg (n=154) |
|
| Men only | |||||
| Anorgasmia | 0 | 0 | 3 | 5 | 8 |
| Libido decreased | 1 | 4 | 5 | 6 | 3 |
| Orgasm abnormal | 0 | 0 | 1 | 2 | 3 |
| Ejaculation delayed | <1 | 1 | 5 | 7 | 6 |
| Erectile dysfunction | 1 | 3 | 6 | 8 | 11 |
| Ejaculation disorder | 0 | 0 | 1 | 2 | 5 |
| Ejaculation failure | 0 | 1 | 0 | 2 | 2 |
| Sexual dysfunction | 0 | 1 | 0 | 0 | 2 |
| PRISTIQ | |||||
| Placebo (n=397) |
50 mg (n=209) |
100 mg (n=267) |
200 mg (n=176) |
400 mg (n=163) |
|
| Women only | |||||
| Anorgasmia | 0 | 1 | 1 | 0 | 3 |
Other adverse reactions observed in premarketing and postmarketing clinical studies
Other infrequent adverse reactions, not described elsewhere in the label, occurring at an incidence of < 2% in MDD patients treated with PRISTIQ were:
Cardiac disorders – Tachycardia.
General disorders and administration site conditions – Asthenia.
Investigations – Weight increased, liver function test abnormal, blood prolactin increased.
Musculoskeletal and connective tissue disorders – Musculoskeletal stiffness.
Nervous system disorders –Syncope, convulsion, dystonia.
Psychiatric disorders – Depersonalization, bruxism.
Renal and urinary disorders – Urinary retention.
Skin and subcutaneous tissue disorders – Rash, alopecia, photosensitivity reaction, angioedema.
In clinical studies, there were uncommon reports of ischemic cardiac adverse reactions, including myocardial ischemia, myocardial infarction, and coronary occlusion requiring revascularization; these patients had multiple underlying cardiac risk factors. More patients experienced these events during PRISTIQ treatment as compared to placebo.
Laboratory, ECG and vital sign changes observed in MDD clinical studies
The following changes were observed in pre-marketing placebo-controlled, short-term MDD studies with PRISTIQ.
Lipids
Elevations in fasting serum total cholesterol, LDL (low density lipoproteins) cholesterol, and triglycerides occurred in the controlled studies. Some of these abnormalities were considered potentially clinically significant.
The percentage of patients who exceeded a predetermined threshold value is shown in Table 4.
| PRISTIQ | |||||
|---|---|---|---|---|---|
| Placebo | 50 mg | 100 mg | 200 mg | 400 mg | |
| Total Cholesterol *(Increase of ? 50 mg/dl and an absolute value of ? 261 mg/dl) |
2 | 3 | 4 | 4 | 10 |
| LDL Cholesterol *(Increase ? 50 mg/dl and an absolute value of ? 190 mg/dl) |
0 | 1 | 0 | 1 | 2 |
| Triglycerides, fasting *(Fasting: ? 327 mg/dl) |
3 | 2 | 1 | 4 | 6 |
Proteinuria
Proteinuria, greater than or equal to trace, was observed in the pre-marketing fixed-dose controlled studies (see Table 5). This proteinuria was not associated with increases in BUN or creatinine and was generally transient.
| PRISTIQ | |||||
|---|---|---|---|---|---|
| Placebo | 50 mg | 100 mg | 200 mg | 400 mg | |
| Proteinuria | 4 | 6 | 8 | 5 | 7 |
Vital sign changes
Table 6 summarizes the changes that were observed in placebo-controlled, short-term, pre-marketing studies with PRISTIQ in patients with MDD (doses 50 to 400 mg).
| PRISTIQ | |||||
|---|---|---|---|---|---|
| Placebo | 50 mg | 100 mg | 200 mg | 400 mg | |
| Blood pressure | |||||
| Supine systolic bp (mm Hg) | -1.4 | 1.2 | 2.0 | 2.5 | 2.1 |
| Supine diastolic bp (mm Hg) | -0.6 | 0.7 | 0.8 | 1.8 | 2.3 |
| Pulse rate | |||||
| Supine pulse (bpm) | -0.3 | 1.3 | 1.3 | 0.9 | 4.1 |
| Weight (kg) | 0.0 | -0.4 | -0.6 | -0.9 | -1.1 |
Treatment with PRISTIQ at all doses from 50 mg per day to 400 mg per day in controlled studies was associated with sustained hypertension, defined as treatment-emergent supine diastolic blood pressure (SDBP) ?90 mm Hg and ?10 mm Hg above baseline for 3 consecutive on-therapy visits (see Table 7). Analyses of patients in PRISTIQ pre-marketing short-term controlled studies who met criteria for sustained hypertension revealed a consistent increase in the proportion of patients who developed sustained hypertension. This was seen at all doses with a suggestion of a higher rate at 400 mg per day.
| Treatment Group | Proportion of Patients with Sustained Hypertension |
|---|---|
| Placebo | 0.5% |
| PRISTIQ 50 mg per day | 1.3% |
| PRISTIQ 100 mg per day | 0.7% |
| PRISTIQ 200 mg per day | 1.1% |
| PRISTIQ 400 mg per day | 2.3% |
Orthostatic hypotension
In the pre-marketing short-term, placebo-controlled clinical studies with doses of 50 to 400 mg, systolic orthostatic hypotension (decrease ?30 mm Hg from supine to standing position) occurred more frequently in patients ?65 years of age receiving PRISTIQ (8%, 7/87) versus placebo (2.5%, 1/40), compared to patients <65 years of age receiving PRISTIQ (0.9%, 18/1,937) versus placebo (0.7%, 8/1,218).
The following adverse reaction has been identified during post-approval use of PRISTIQ. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure:
Skin and subcutaneous tissue disorders – Stevens-Johnson syndrome.
Gastrointestinal disorders – Pancreatitis acute.
Link to the Full Document on Manufacturer Page

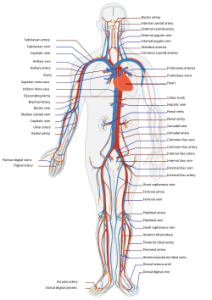
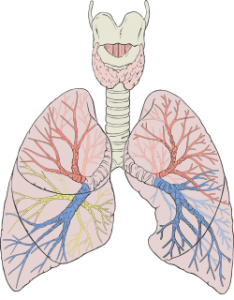
Using morphine can cause both reversible and permanent changes to the body. In fact, morphine affects almost all systems and organs in the human body, and excessive or prolonged use can bring dangerous consequences.
However, the greatest risk of using morphine is death resulting from the gradual shutdown of the respiratory system.
What are some of the benign or even the more serious effects of morphine on the body? We examine here. 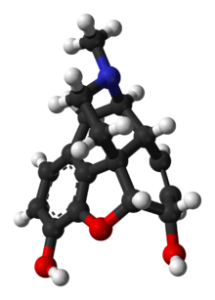
Finally, it is important to note that using morphine for longer than a week or two can lead to dependence. When you become dependent on morphine, you experience withdrawal symptoms when you lower or cease dosing. With use over time, morphine also causes tolerance…meaning that more of the drug is needed in order to be effective.
Image credit: wikipedia.org

Highlights of side effects are listed here link to Manufacturer found at bottom of post – I highly recommend you study each and every detail, use google and youtube to find stories that are not included in the official report.
Seizure
If you take XTANDI you may be at risk of having a seizure. Avoid activities where losing consciousness could seriously harm you or someone else. Tell your doctor right away if you lose consciousness or have a seizure. Your doctor will stop XTANDI if you have a seizure during treatment.
Posterior Reversible Encephalopathy Syndrome (PRES)
If you take XTANDI you may be at risk of developing a condition involving the brain called PRES. Tell your healthcare provider right away if you have a seizure or quickly worsening symptoms such as headache, decreased alertness, confusion, reduced eyesight, blurred vision or other visual problems. Your healthcare provider will do a test to check for PRES. Your healthcare provider will stop XTANDI if you develop PRES.
XTANDI may cause infections, falls and injuries from falls. Tell your doctor if you have signs or symptoms of an infection or if you fall.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of XTANDI. For more information, ask your healthcare provider or pharmacist.
Download the official PDF http://www.astellas.us/docs/us/12A005-ENZ-WPI.pdf
Page [tcb_pagination_current_page] of [tcb_pagination_total_pages]